Financial Assistance Plain Language Summary
Teton Valley Health Care (TVHC) cares for the healthcare needs of you and your loved ones, regardless of your ability to pay. We will work with you to determine if you qualify for financial assistance. If you are having trouble paying for your health care needs at one of TVHC’s facilities, please contact one of our Patient Financial Advocates at 208-354-6320.
· Medically necessary medical services may be free or discounted based on how your income compares to federal poverty guidelines.
· You can apply for financial assistance by calling one of our Patient Financial Advocates at 208-354-6320.
· Financial Assistance applications can be found on our website.
· If you are without insurance, we can assist you in applying for programs such as Medicaid.
· Our discounts are determined using a method called Amounts Generally Billed (AGB). This process is compliant with the IRS 501r regulations.
· If you find it hard to pay your balance in full, we offer interest-free payment plans to ease the financial burden. To set up a payment plan, please contact one of our Patient Financial Advocates at 208-354-6320.
Financial Assistance Application (English) – 2024
Financial Assistance Application (Spanish) – 2024
Policy:
It is the policy of Teton Valley Health Care (TVHC) to be a community health care organization guided by a commitment to its Mission and Core Values. It is both the philosophy and practice of our district that medically necessary health care services are available to community members and those in emergent medical need, without delay, regardless of their ability to pay. TVHC will follow the guidelines listed below:
- Comply with federal and state laws and regulations relating to emergency medical services and financial
- Provide financial assistance to qualifying patients with no other third-party payment sources to relieve them of all or some of their financial obligation for medically necessary health care services.
- In alignment with its Core Values, TVHC will provide financial assistance to qualifying patients in a respectful, compassionate, fair, consistent, effective and efficient manner.
- Not discriminate based on age, sex, race, creed, color, disability, sexual orientation, national origin, religion, gender identity or immigration status when making financial assistance determinations.
- In extenuating circumstances, TVHC may, at our discretion, approve financial assistance outside of the scope of this
Financial assistance is not considered to be a substitute for personal responsibility. Patients are expected to cooperate with TVHC’s requirements for obtaining financial assistance or other forms of payment. Patients who do not cooperate in the process may result in ineligibility of financial assistance.
Definition:
Financial Assistance means “medically necessary hospital health care rendered to indigent persons when third-party coverage, if any, has been exhausted, to the extent that the person(s) is unable to pay for the care or to pay their deductible or coinsurance amounts required by a third-party payer, based on the criteria in this policy and procedure.”
Third-Party coverage means “an obligation on the part of an insurance company, health care service contractor, health maintenance organization, group health plan, government program (Medicare, Medicaid or medical assistance programs, workers compensation, veteran benefits, tribal health benefits or health care sharing ministry as defined in 216 U.S.C. Sec. 5000A) to pay for the care of covered patients and services, and may include settlements, judgments or awards actually received related to the negligent acts of others (for example, auto accidents or personal injuries) which have resulted in the medical condition for which the patient has received hospital health care services.”
Prima-Facie: “What is known based on first appearance but is subject to further evidence or information.”
Medically Indigent: A patient, whose health insurance coverage, if any, does not provide full coverage for their medical expenses and that their medical expenses, in relationship to their income, would make them indigent if they were forced to pay full charges for their medical expenses.
Federal Poverty Guideline and Thresholds
- Guidelines are the federal poverty measurement issued by the Department of Health and Human Services and issued in the Federal Register which is applicable to TVHC.
- Thresholds are the original version of the Federal Poverty measurement and are used by the Census Bureau for statistical purposes only and not applicable to TVHC.
Family-is defined as a group of two people or more (one whom is the householder) related by birth, marriage, or adoption and residing together. All such people, including related subfamily members, are considered members of one family.
Income includes earnings, unemployment compensation, workers’ compensation. Social Security, supplemental security income, public assistance, Veteran’s payments, survivor benefits, pension or retirement income, interest, dividends, rents, royalties, income from estates, trusts, educational assistance, alimony, child support, assistance from outside the household and other miscellaneous sources.
Purpose:
The purpose of this policy and procedure is to outline the circumstances under which financial assistance discounts may be provided to qualifying low-income patients for medically necessary health care services provided by TVHC and its owned ambulatory outpatient clinics.
Procedure:
1. Eligibility Criteria:
Services: The following health care services are eligible for financial assistance:
- Financial assistance is granted for medically necessary services TVHC recognizes appropriate hospital based services as defined as “those hospital services which are reasonably calculated to diagnose, correct, cure, alleviate, or prevent the worsening of conditions that endanger life, or cause suffering or pain, or result in illness or infirmity, or threaten to cause or aggravate a handicap, or cause physical deformity or malfunction, and there is no other equally effective more conservative or substantially less costly course of treatment available or suitable for the person requesting the service. For the purpose of this section, “course of treatment” may include mere observation or, where appropriate, no treatment at all. This policy also applies to clinic and physician services for medically necessary services excluding those charges to which the clinic sliding scale applies.
- Patients who reside outside the TVHC defined area are not eligible for financial assistance, except under extenuating circumstances which may include emergent services while visiting our hospital service area and meets the eligibility requirements outlined in this policy.
- Elective and preventative procedures and services are ineligible for financial
- TVHC will provide free or discounted hospital services to qualified low income, uninsured and underinsured patients, when the ability to pay for services is a barrier to accessing medically necessary services. Patients must meet the requirements outlined in this policy.
2. Eligibility for Financial Assistance:
Financial assistance is secondary to all other financial resources available to the guarantor including but not limited to insurance, third party liability payers, government programs and outside agency programs. In situations where appropriate primary payment sources are not available, guarantors may apply for financial assistance based on the eligibility requirements in this policy.
The TVHC service area is defined as East Teton County, from Felt, ID to the west, eastward to the WY border. In addition, the postal zip code area of Alta, WY (zip code 83414) to the extent that this area extends beyond Teton County.
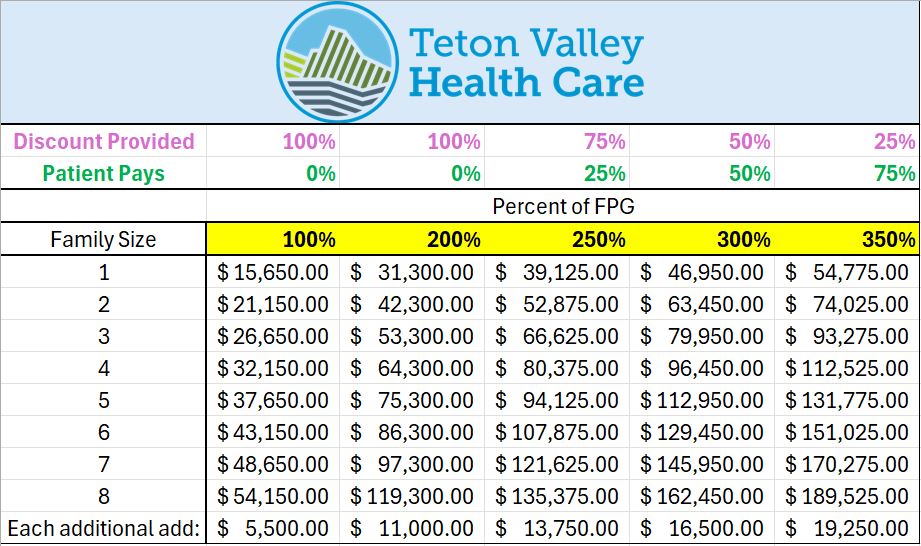
- The full amount (100%) of hospital charges will be adjusted as financial assistance for any guarantor whose gross family income is at or below 100% of the current federal poverty guideline level, provided that such persons are not eligible for other private or public health coverage sponsorship.
- The TVHC sliding fee scale will be used to determine the amount to be written off as financial assistance for guarantors with incomes between 100% and 350% of the current federal poverty level. This is applicable after all funding possibilities available to the guarantor have been exhausted or denied and personal financial resources have been reviewed for possible funding to pay for services and supplies The sliding scale is listed below. The decision to provide Financial Assistance is based solely on family size and gross income. Assets are not used in the determination of financial assistance.
- This policy is applicable for all emergent services in all service areas including primary care services, Rural Health Clinic services, emergency room, outpatient, and inpatient services.
- Limitations on Charges: Amounts Generally Billed (AGB) are used to determine the minimum discount amount that will be offered to underinsured and uninsured patients who qualify for financial The AGB is determined by looking at all billed and paid claims from the prior year. The net payment amount is used to determine the average payment amount per financial class. The AGB calculation is used to determine the minimum discount for the following calendar year.
Eligibility for financial assistance shall be based on financial need at the time of the application date unless looking back more than 24 months. If we look back more than 24 months, we will base the financial need on the patient/guarantor’s income and family size during the specified date of service. All resources of the family are considered in determining the applicability of the TVHC sliding fee scale. Calculation of the applicable financial assistance discount is based on current Federal Poverty Guidelines. The rate table and discount percentages are listed below.
Eligibility on a completed application is valid for eligible services received within the subsequent ninety (90) days from the application approval date. If assistance is still needed at the end of the 90 days, the patient/guarantor can reapply.
3. Medicaid and Health Benefit Exchange Obligations:
Identification of Patients Eligible for Certain Third-Party Coverage
- For services provided to patients on or after October 1, 2022, the following procedure will apply for identifying patients and/or their guarantors who may be eligible for health care coverage through Idaho Medical Assistance programs (e.g., Medicaid).
- As part of the Financial Assistance Program application process for determining eligibility for financial assistance, TVHC will query the patient as to whether they meet the criteria for health care coverage under the financial assistance
- If information in the financial assistance application indicates that the patient or their guarantor may be eligible for coverage, TVHC will assist the patient or their guarantor in applying for coverage under these Per each patient’s needs, this includes walking them through the process, answering questions, providing them with the appropriate forms, linking them to an agency representative and/or providing them with the appropriate links.
- The assistance offered to patients or guarantors may TVHC will take into account any physical, mental, intellectual, sensory deficiencies, lack of access to a computer/internet, language barriers and any other reason that may constitute an unreasonable burden.
- If the patient or guarantor fails to make reasonable efforts to cooperate with TVHC, in applying for coverage, TVHC is not obligated to provide financial assistance to such patient.
- If a patient or their guarantor is obviously or categorically ineligible or has been deemed ineligible for coverage through financial assistance programs in the prior 12 months, TVHC will not require the patient or their guarantor to apply for such coverage.
4. Eligibility Determination Process:
- Financial assistance forms, instructions and written applications shall be furnished to patients when financial assistance is requested, when a need is indicated or when financial screening indicates potential need. All applications, whether initiated by the patient, hospital, clinic or other means, will be accompanied by documentation to verify the family income amount indicated on the application form. Prima-facie write-offs are an exception.
- As part of this screening process, TVHC and our outsourced early out self-pay vendor will review whether the guarantor has exhausted or is not eligible for any third-party payment Where the patient/guarantor’s identification as an indigent person is obvious to TVHC via a prima-facie determination of eligibility, TVHC may voluntarily initiate the financial assistance process, which may not require an application or supporting documentation. All prima-facie determinations require approval by the hospital Revenue Cycle Director and CFO and will be documented in the electronic health record.
- A guarantor who may be eligible to apply for financial assistance after the initial screening will be given fourteen (14) days or such time as may be reasonably necessary to provide documentation to TVHC to support a charity/financial assistance determination. Based upon documentation provided with the application, TVHC will determine if additional information is required, or whether a determination can be made. Failure of a guarantor to reasonably complete appropriate application procedures shall be sufficient grounds for TVHC to deny assistance and to initiate outside collection efforts which may include garnishments, legal action and other legal means for securing payment.
- An initial determination of potential eligibility for financial assistance will be completed as closely as possible to the date of service or upon request by or on behalf of the patient.
Any one or a combination of the following documents shall be considered sufficient evidence upon which to base the final determination of financial assistance eligibility:
- W-2 withholding
- Pay stubs from all employment during the relevant time
- Income tax return from the most recently filed calendar
- Forms approving or denying eligibility for Medicaid and or state-funded medical
- Forms approving or denying unemployment compensation; or
- Written statement from employers or DSHS employees
NOTE: Additional information may be requested if the documentation does not support the patient’s financial assistance application. For example, for seasonal workers, a W2 income tax return may not be requested, and pay-stubs alone may be used in order to ensure proper rating of the patient.
Household – Family size is considered in the determination. TVHC further clarifies the definition of family size (related by blood, marriage, adoption) to include a family as parents, children and other members of the household that are claimed as dependents on federal income taxes for the most recently filed return. (e.g., If an adult child files their own taxes but lives in the home, TVHC will not look at the parents’ income to evaluate their financial application.)
- If the responsible party is not able to provide any of the documentation described above, the hospital shall rely upon written and signed statements from the responsible party for making a final determination of eligibility for classification as an indigent
- TVHC will make available to the patient/guarantor a designated representative to assist the patient in completing the Financial Assistance
- All information relating to the application will be kept Copies of documents that support the application will be kept with the application form. Documents will be retained for six (6) years. After six years, documents may be destroyed. They are non-archival, nonessential.
- TVHC will notify the patient/guarantor, in writing, of the final determination within fourteen (14) business days of receiving all necessary documentation. The determination of eligibility can be made at any time upon learning that a responsible party’s income is below 350% of the
- The guarantor may appeal the determination of ineligibility for financial assistance by providing relevant additional documentation to TVHC within thirty (30) days from the date of the TVHC will not refer the account to an external collection agency within these 30 days. If the account has already been assigned to an outside collection agency, the hospital’s business office will request a hold be placed on the account until a decision is made. After the thirtieth day, if no appeal has been filed, the hospital may initiate or resume collection activities. The patient must contact our early out vendor; (Kinum) at 1-888-471-0280 or TVHC’s billing department at 208-354-6345-to appeal a denial of financial assistance.
- All appeals will be reviewed and if the determination on appeal affirms the denial, written notification will be sent to the guarantor and the Department of Health, where required, in accordance with state The final appeal process will conclude within thirty (30) days from the date of the original denial.
5. Reporting:
TVHC shall report data to appropriate State and Federal agencies if required, Data may include the amount of charity/financial assistance provided. The collection agencies shall submit to TVHC’s Revenue Cycle Director, an annual summary report on collection actions taken. These documents will be reviewed annually with the Finance Committee.
6. Refunds:
In the event that the patient/guarantor pays a portion, or all of the charges related to appropriate hospital-based medical care services and is subsequently found to have met the financial assistance criteria, any payments in excess of the amount determined to be appropriate shall be refunded to the patient within thirty days of achieving the eligibility designation.
7. Training:
TVHC shall provide regular, standardized training to all pertinent staff regarding the hospital’s financial assistance policy. Appropriate staff consists of registration, admissions, billing, clinics and may include other areas and departments. (i.e., Case Management, Utilization Review, Quality etc.).
8. Billing and Collections:
Any unpaid balances owed by the patient/guarantor, after the financial assistance application is reviewed and any applicable adjustments applied, the patient/guarantor may set up a payment plan for all balances due (if any). Failure to adhere to the agreed upon payment plan may result in the balance being assigned to an outside collection agency.
9. Communication of Financial Assistance:
- TVHC will prominently display the notice of financial assistance in all primary spoken languages, in areas where patients are admitted or registered including the emergency department.
- A current version of this policy, a plain language summary, the financial assistance form, and directions on how to complete the form, will be posted on our hospital website in English and the second most spoken language in our area, which is Spanish.
- Language pertaining to financial assistance will be prominently displayed on the first page of each patient statement in both English and Spanish.
- For other languages, TVHC will work with an external vendor to produce these documents in the preferred language upon
10. Sliding Scale Fee: